Medical device and MedTech insights, news, tips and more
Seven Areas in a Hospital that Could Cause Healthcare Acquired Infections
June 6, 2016
Healthcare acquired infections (HAIs) are the third leading cause of death in the US, behind heart disease and cancer. One in every 25 inpatients will acquire an infection while being treated. These infections lead to the loss of tens of thousands of lives and cost billions of dollars every year. Since these infections are largely preventable, the federal government has added significant penalties to facilities with high infection rates. The pressure is on to address this issue now.
Foundational Issue:
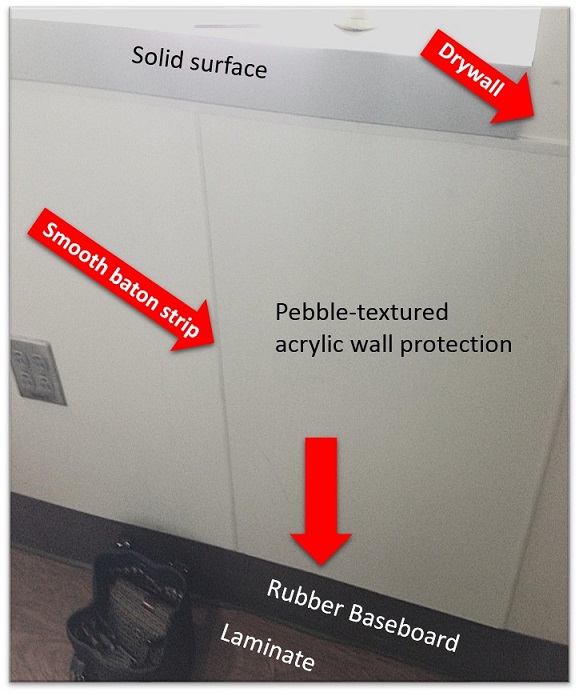
The science of surfaces as a fomite (object or material that is likely to carry infection) is just now maturing. Research has shown that microbes can live on “clean and disinfected” surfaces for days, weeks and even months. How is this possible when surfaces are being regularly cleaned and disinfected? The goal of this article is to present seven aspects of surface selection and to gain an understanding of why facilities must set surface criteria to not only minimize financial risk, but also to prevent harm to patients, healthcare workers and the general public.
Surfaces are a complicated subject. Most people think of surfaces as part of the design and construction process and not as part of an infection prevention and control program. When selecting materials, a lot of focus tends to be given to colours and textures that create “a healing environment.” Although these aspects of a surface material are certainly important, there are many other surface properties that are of critical importance, yet are not thought about or given proper evaluation. In order for an environment to be “healing” it need to also not introduce the potential for detrimental effects, like infections. After all, the most soothing colour and texture is of little value to a surface that cannot be cleaned or disinfected properly.
People interact with surfaces throughout the day without a second thought. If hands are washed regularly, a person with a healthy immune system has a good chance of reducing his risk of infection. This is not necessarily true for someone with a compromised immune system.
Ironically, surfaces are often cleaned and disinfected based on visual inspection, even though it is commonly understood that microbes cannot be seen. Research has shown that at the microscopic level, microbe counts can quickly rebound, often times to levels seen prior to cleaning and disinfection. This leaves patients, healthcare workers and the general public at constant risk of acquiring and spreading infection. In fact, studies show that patients are at risk of contracting an infection, such as MRSA or C. Difficilie from the patient who previously occupied the same room at a rate of 35% to 50%, depending on the infection, despite routine and terminal cleaning and disinfection.
Read More – Source: Seven Aspects of Surface Selection in Healthcare
